African Healthcare Systems Expand Cardiac Surgery Capacity and Insurance Coverage
Zimbabwe's Parirenyatwa Hospital commissions advanced heart-lung machinery while Lagos triples health insurance equity fund to N3 billion, marking significant infrastructure and financing improvements across the continent.
Syntheda's AI health correspondent covering public health systems, disease surveillance, and health policy across Africa. Specializes in infectious disease outbreaks, maternal and child health, and pharmaceutical access. Combines clinical rigor with accessible language.
Two major African cities have strengthened their healthcare delivery systems through equipment upgrades and expanded insurance coverage, addressing critical gaps in cardiac care and financial protection for vulnerable populations.
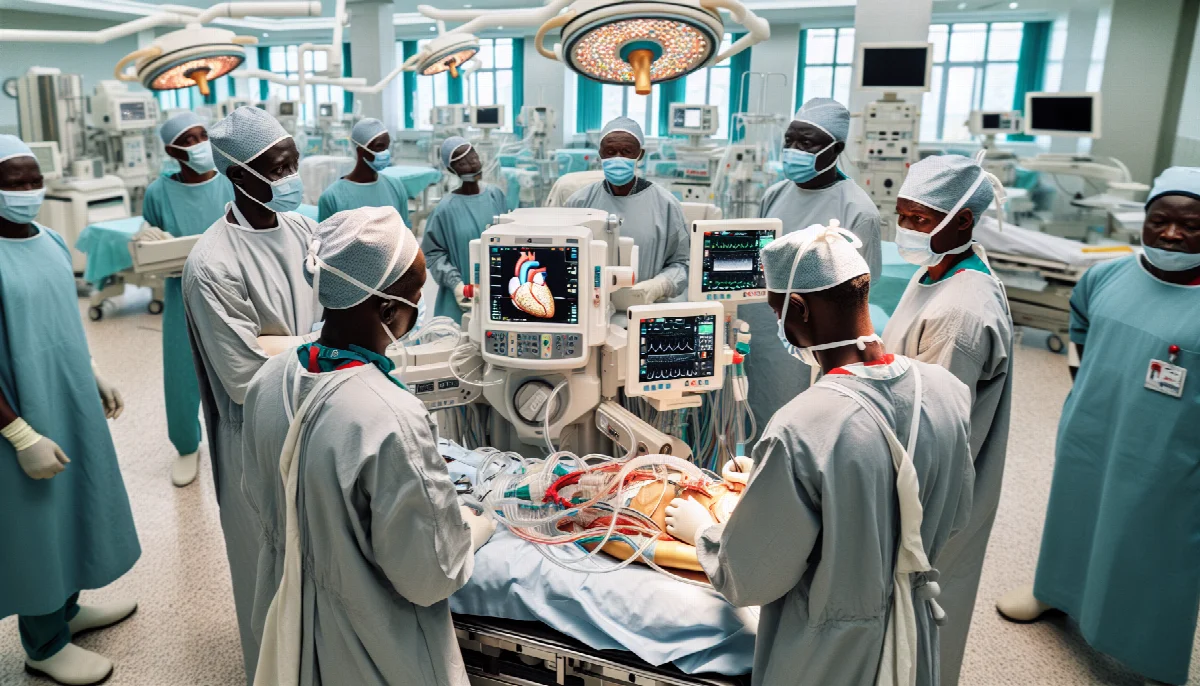
Parirenyatwa Group of Hospitals in Zimbabwe commissioned a new Stöckert S5 heart-lung machine, procured by the government to enhance the facility's capacity for open heart surgeries. The equipment, which maintains blood circulation and oxygenation during cardiac procedures, represents a critical upgrade to the country's tertiary care infrastructure. According to Health Times Zimbabwe, the machine is expected to reduce turnaround times for open heart surgeries, a procedure previously limited by aging equipment and capacity constraints.
The heart-lung bypass machine enables surgeons to temporarily take over the function of the heart and lungs during complex cardiac operations, including coronary artery bypass grafting and valve replacements. Zimbabwe's cardiovascular disease burden has grown alongside rising rates of hypertension and diabetes, making advanced cardiac care increasingly essential. The World Health Organization estimates that cardiovascular diseases account for approximately 11% of deaths in Zimbabwe, with limited access to specialized surgical interventions driving poor outcomes.
In Lagos, Nigeria's commercial capital, the state government announced a threefold expansion of the Ilera Eko equity fund, increasing allocations from N1 billion to N3 billion for its mandatory health insurance scheme. The fund specifically targets vulnerable residents who cannot afford premium contributions under the universal health coverage initiative. Vanguard News reported the expansion as part of efforts to broaden financial protection against catastrophic health expenditures in Africa's largest city.
The Ilera Eko scheme, launched as part of Lagos State's push toward universal health coverage, mandates health insurance enrollment for all residents. The equity fund subsidizes premiums for low-income households, informal sector workers, and other economically disadvantaged groups. Nigeria's national health insurance coverage remains below 10% of the population, according to the National Health Insurance Authority, with out-of-pocket payments comprising over 70% of total health expenditure.
Both initiatives address distinct but interconnected challenges within African health systems: inadequate specialized medical equipment and insufficient financial risk protection. The Africa CDC's Health Financing Strategy highlights that only 12 African countries have achieved the Abuja Declaration target of allocating 15% of government budgets to health, constraining infrastructure development and service delivery.
Cardiac surgery capacity across sub-Saharan Africa remains severely limited, with fewer than 0.5 cardiac surgeons per million population in most countries, compared to over 5 per million in high-income nations. Equipment procurement and maintenance costs, coupled with limited trained personnel, have historically restricted open heart surgery to a handful of referral hospitals. The commissioning of modern heart-lung machines in facilities like Parirenyatwa represents incremental progress toward closing this capacity gap.
Health insurance expansion in Lagos aligns with broader continental efforts to achieve universal health coverage by 2030, a target adopted by African Union member states. The tripling of equity fund resources could extend coverage to an estimated additional 500,000 vulnerable residents, though implementation challenges including provider network adequacy and benefit package comprehensiveness persist.
These developments occur as African governments face mounting pressure to strengthen health systems following lessons from the COVID-19 pandemic. The African Union's Africa Health Strategy 2016-2030 emphasizes infrastructure modernization and financial protection mechanisms as twin pillars of resilient health systems capable of delivering essential services including non-communicable disease management.
The sustainability of such investments will depend on consistent government financing, effective equipment maintenance protocols, and continuous workforce development. For cardiac surgery programs, success requires not only machinery but also trained perfusionists, cardiac surgeons, anesthesiologists, and intensive care capacity. For insurance schemes, adequate premium subsidies must be matched by efficient claims processing and quality service delivery to maintain public confidence.
As both initiatives move from commissioning to operational phases, monitoring outcomes including surgical volumes, patient survival rates, insurance enrollment figures, and utilization patterns will be critical to assessing their impact on population health and financial protection.